|
Review Article
Impacts of novel pandemic coronavirus (COVID-19) outbreak on dental practice: A review of the current literature
1 Department of Oral and Maxillofacial Medicine, Shar Teaching Hospital, Sulaymaniyah, Kurdistan Region, Iraq
2 Department of Oral and Maxillofacial Surgery, School of Medicine, Faculty of Dental Sciences, University of Sulaimani, Al Sulaymaniyah, Kurdistan, Iraq
3 Department of Medical Laboratory Sciences, Charmo University, 46023 Chamchamal, Sulaimani, Kurdistan Region, Iraq
Address correspondence to:
Shakhawan M Ali
Department of Oral and Maxillofacial Surgery, School of Medicine, College of Dentistry, University of Sulaimani, Sulaymaniyah, Kurdistan Region,
Iraq
Message to Corresponding Author
Article ID: 100040D01PM2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Mahmud PK, Ali SM, Sabir DK. Impacts of novel pandemic coronavirus (COVID-19) outbreak on dental practice: A review of the current literature. Edorium J Dent 2020;7:100040D01PM2020.ABSTRACT
The World Health Organization announced that the outbreaks of the novel coronavirus have constituted a public health emergency of international concern. The epidemic of coronavirus disease 2019 (COVID-19), originating in Wuhan, China, has become a major public health challenge for not only China but also for countries around the world. As for April 12, 2020, COVID-19 has been recognized in almost all the countries around the globe, with a total of 1,696,588 laboratory-confirmed cases and 105,952 deaths. Inhalation or contact with infected droplets is the main rout of disease transmission and the incubation period ranges from 2 to 14 days. Fever, cough, sore throat, breathlessness, fatigue, malaise are the symptoms of the disease. In most people the disease is mild or asymptomatic but in some (usually the elderly and those with comorbidities) the disease is fatal because of progress to pneumonia, acute respiratory distress syndrome (ARDS), and multi-organ dysfunction. Urgently infection control measures are necessary to prevent the virus from further spreading and to help control the epidemic situation. One of the characteristics of dental settings is the risk of cross infection can be high between patients and dental practitioners due to the face-to-face communication and the exposure to handling of sharp instruments, saliva, blood, and other body fluids. Staff of dental clinics and hospital plays great roles in preventing the transmission of COVID-19 disease. We strongly recommended all elective and nonessential dental services are immediately must be suspended only emergency treatment should continue with infection control measures during dental practice to block the person-to-person transmission routes in hospitals and dental clinics.
Keywords: Coronavirus infections, COVID-19 disease, Dentistry, Infection control, Pandemic, Pneumonia
INTRODUCTION
Severe acute respiratory syndrome corona virus 2 (SARS-CoV-2) is etiological agent of the severe acute respiratory syndrome corona virus disease 2019 (COVID-19). The disease was initially identified in the Wuhan city of Hubei Province of China and now it has infected almost all the countries around the world [1]. World Health Organization declared a public health emergency of international concern over this global pneumonia outbreak on 30th January 2020 [2]. The patients who suffered from the novel viral pneumonia typical clinical symptoms were fever, cough, and myalgia or fatigue with abnormal chest computed tomography (CT) scan, also sputum production, headache, hemoptysis, and diarrhea are the less common symptoms [3],[4],[5]. As of April 12, COVID-19 has been worldwide pandemic and recognized in most countries, with a total of 1,696,588 laboratory-confirmed cases and 105,952 deaths [6]. The risk of cross infection may be high between dental practitioners and patients due to the characteristics of dental settings. Dental practices and hospitals in countries/regions that are (potentially) affected with COVID-19, strict and effective infection control protocols are needed urgently [7]. Based on relevant guidelines and research, this review article introduces the essential knowledge about COVID-19 and infection control measures during dental practice to reduce the possibility of person-to-person transmission routes in dental clinics and hospitals during this outbreak.
CHARACTERISTICS OF SARS-COV-2
SARS-CoV-2 is a betacoronavirus in the same subgenus as the severe acute respiratory syndrome (SARS) virus (as well as several bat coronaviruses), but in a different clade. Full-genome sequencing and phylogenic analysis indicated that the coronavirus that causes new disease has the structure of the receptor-binding gene region which is very similar to the SARS coronavirus, and the virus has been shown to use the same receptor, the angiotensin-converting enzyme 2 (ACE2), for cell entry [8]. The Coronavirus Study Group of the International Committee on Taxonomy of viruses has proposed that this virus be designated severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [9]. Another betacoronavirus appears more distantly related to the Middle East respiratory syndrome (MERS) virus [10],[11]. The closest RNA sequence similarity is to two bat coronaviruses, and it appears likely that bats are the primary source, whether COVID-19 virus is transmitted directly from bats or through some other mechanism (e.g., through an intermediate host) is unknown [12]. Two different types of SARS-CoV-2 were identified among 103 strains of SARS-CoV-2 from China in a phylogenetic analysis, designated type L (accounting for 70% of the strains) and type S (accounting for 30%) [13]. The L type was predominated during the early days of the epidemic in China, but accounted for a lower proportion of strains outside of Wuhan than in Wuhan until now the clinical implications of these findings are uncertain.
TRANSMISSION ROUTES OF COVID-19
The COVID-19 transmission routes currently are still to be determined, but human-to-human transmission has been confirmed [14],[15]. The main source of transmission is symptomatic COVID-19 patient, although recent observations suggest that asymptomatic patients and patients in their incubation period are also carriers of SARS-CoV-2 and who have been the source of transmission [16],[17]. The incubation period of SARS-CoV-2 has been estimated at 5 to 6 days on average, but there is evidence that it could be as long as 14 days, which is now the commonly adopted duration for medical observation and quarantine of (potentially) exposed persons [18],[19]. Also it is difficult to identify and quarantine these patients in time because epidemiologic feature of COVID-19 has made it control extremely challenging and the result leads to accumulation of SARS-CoV-2 in communities [2]. More than that, it remains to be proved whether patients in the recovering phase are a potential source of transmission [17]. The transmission of COVID-19 has been described by several potential scenarios such as the transmission via contact with droplets from talking, coughing, sneezing (related to human respiratory activities), contact transmission (contact with oral, nasal, and eye mucous membranes), and aerosols generated during clinical procedures are expected, as it would be for other respiratory infections. The droplets can be nasopharyngeal or oropharyngeal origin, normally associated with saliva droplets could contribute to viral transmission to subjects nearby, and, on the other side, the long-distance transmission is possible with smaller droplets infected with air-suspended viral particles [20]. Notable case report regarding COVID-19 infection in Germany shows that transmission of the virus may also be occurred through contact with asymptomatic patients [17]. New studies have suggested that COVID-19 may be airborne through aerosols formed during medical procedures [21]. Conspicuous study shows that SARS-CoV-2 RNA could also be detected by reverse transcription polymerase chain reaction (RT-PCR) testing in a stool specimen collected on day 7 of the patient’s illness [22].
CLINICAL MANIFESTATIONS
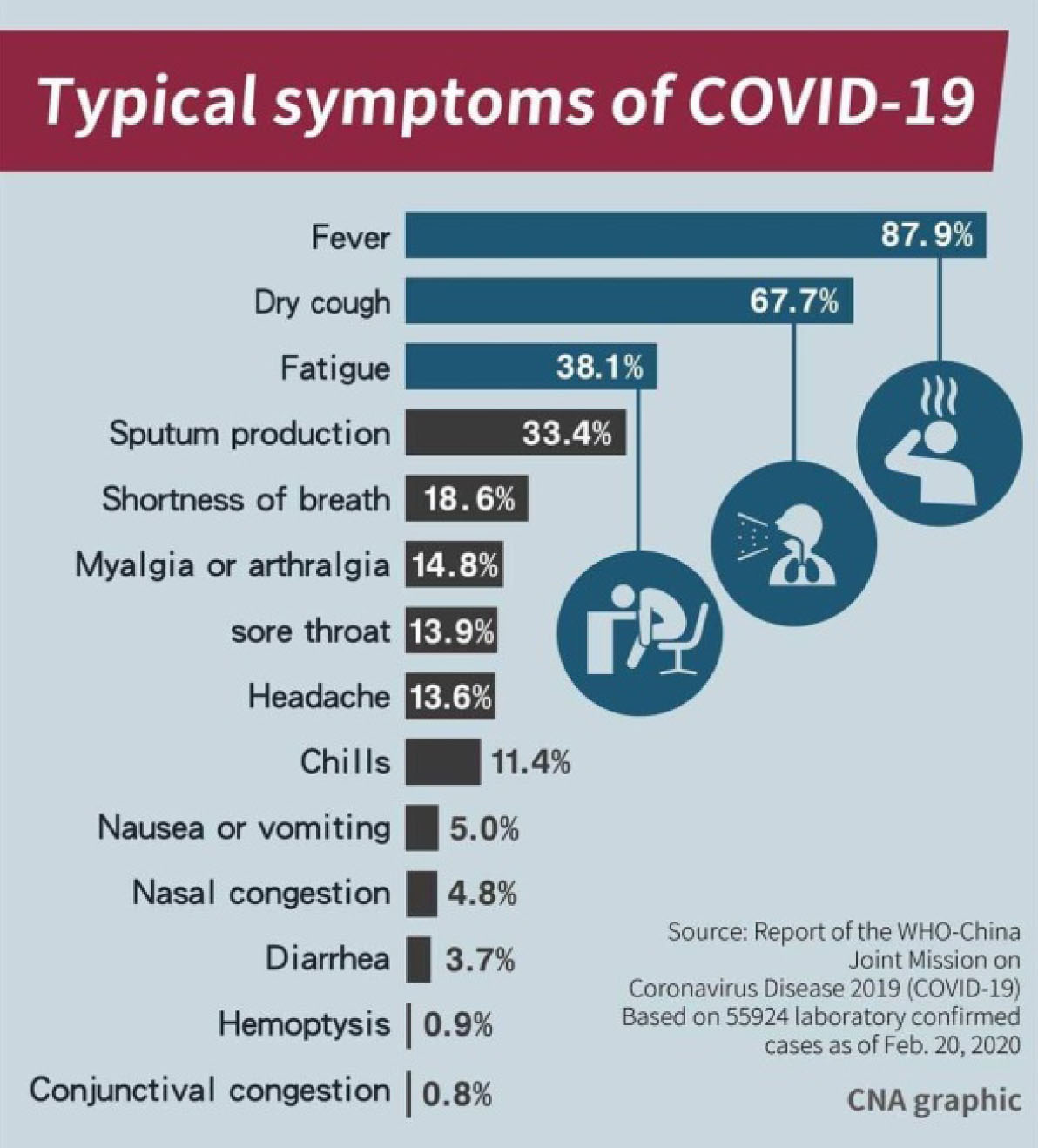
Clinically the majority of patients with COVID-19 represent relatively mild cases or asymptomatic. According to recent study by Guan et al. (2020) in China hospitals and data from the National Health Commission of China, the proportion of severe cases among all patients with COVID-19 in China was around 15–25% [4]. Typical symptoms fever and dry cough, while some also had shortness of breath, fatigue, and other atypical symptoms, such as muscle pain, confusion, headache, sore throat, diarrhea, and vomiting (Figure 1) [4]. In the most common pattern, patients who underwent chest CT were showed bilateral pneumonia, with ground-glass opacity and bilateral patchy shadows [2],[4]. In general, older age and the existence of underlying comorbidities (e.g., diabetes, hypertension, and cardiovascular disease) were associated with poorer prognosis [23].
DIAGNOSIS AND TREATMENT
A combination of epidemiologic information (e.g., a history of travel to or residence in affected region 14 days prior to symptom onset), clinical symptoms, CT imaging findings, and laboratory tests (e.g., RT-PCR tests on respiratory tract specimens) plays an important role in the diagnosis of COVID-19 according to standards of either the WHO or the National Health Commission of China [24]. Another important point should be mentioned that a single negative RT-PCR test result from suspected patients does not exclude infection. Also we should clinically be alert of patients with an epidemiologic history, COVID-19-related symptoms, and/or positive CT imaging results. Currently, the approach to COVID-19 is to control the source of infection, use infection prevention and control measures to lower the risk of transmission, and provide early diagnosis, isolation, and supportive care for affected patients [5]. Till now no any especial treatment just management of COVID-19 has been largely supportive [24].
THE WORKERS WHO ARE AT THE GREATEST RISK
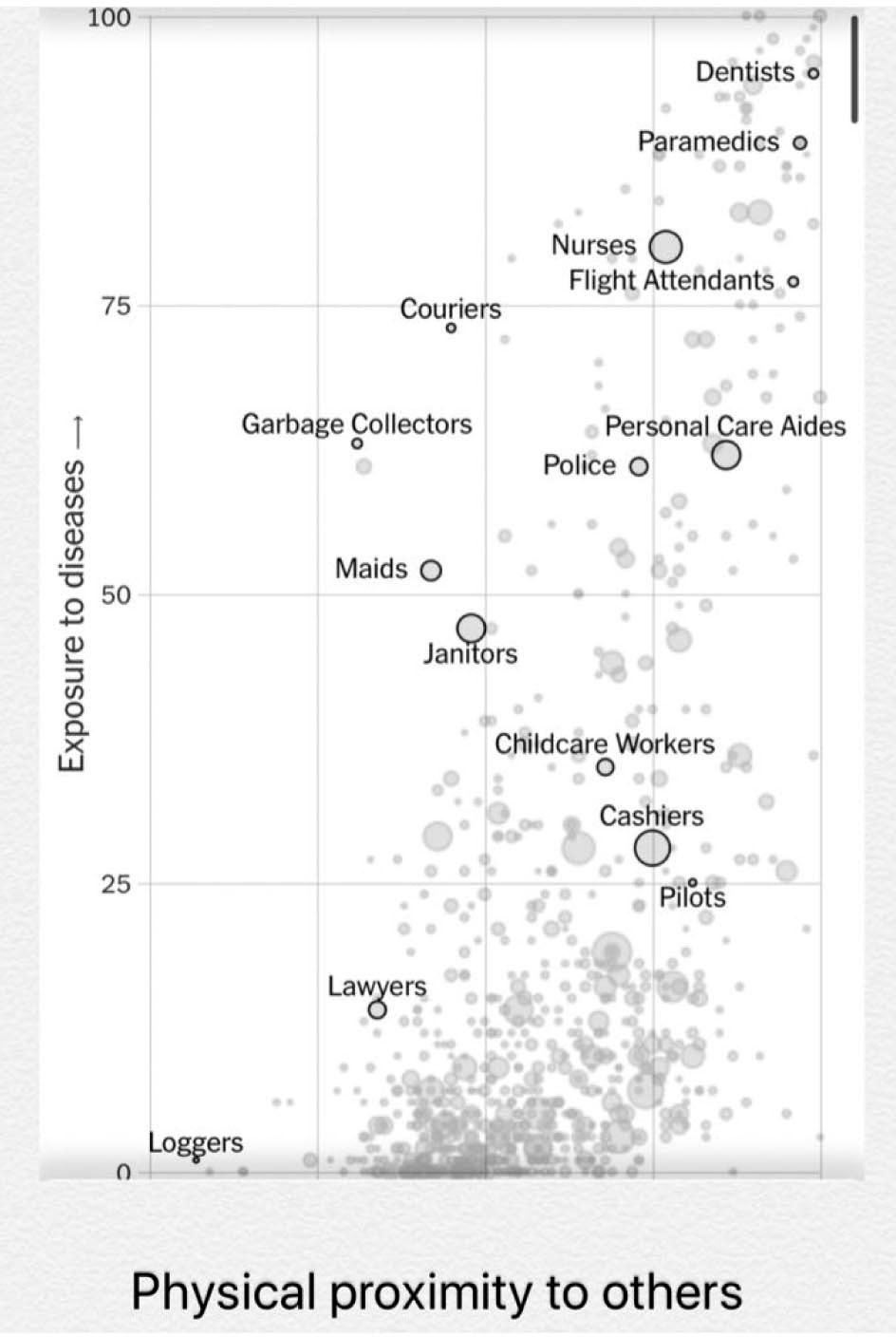
As the coronavirus continues to spread throughout the world, people with jobs that put them in physical contact with many others are at the greatest risk of becoming sick. Health care workers are at the greatest risk as they can encounter diseases and infections daily and typically work in close proximity to one another and their patients. Many are already under quarantine because of exposure to the virus (Figure 2). Now dentists are at the top front to fight against the virus. Horizontal position in the figure shows a measure of how close people are to others during their workdays. On the chart, each bubble represents an occupation. The bigger the bubble, the more people do that job [25].
POSSIBLE TRANSMISSION ROUTES OF COVID-19 IN DENTAL CLINICS
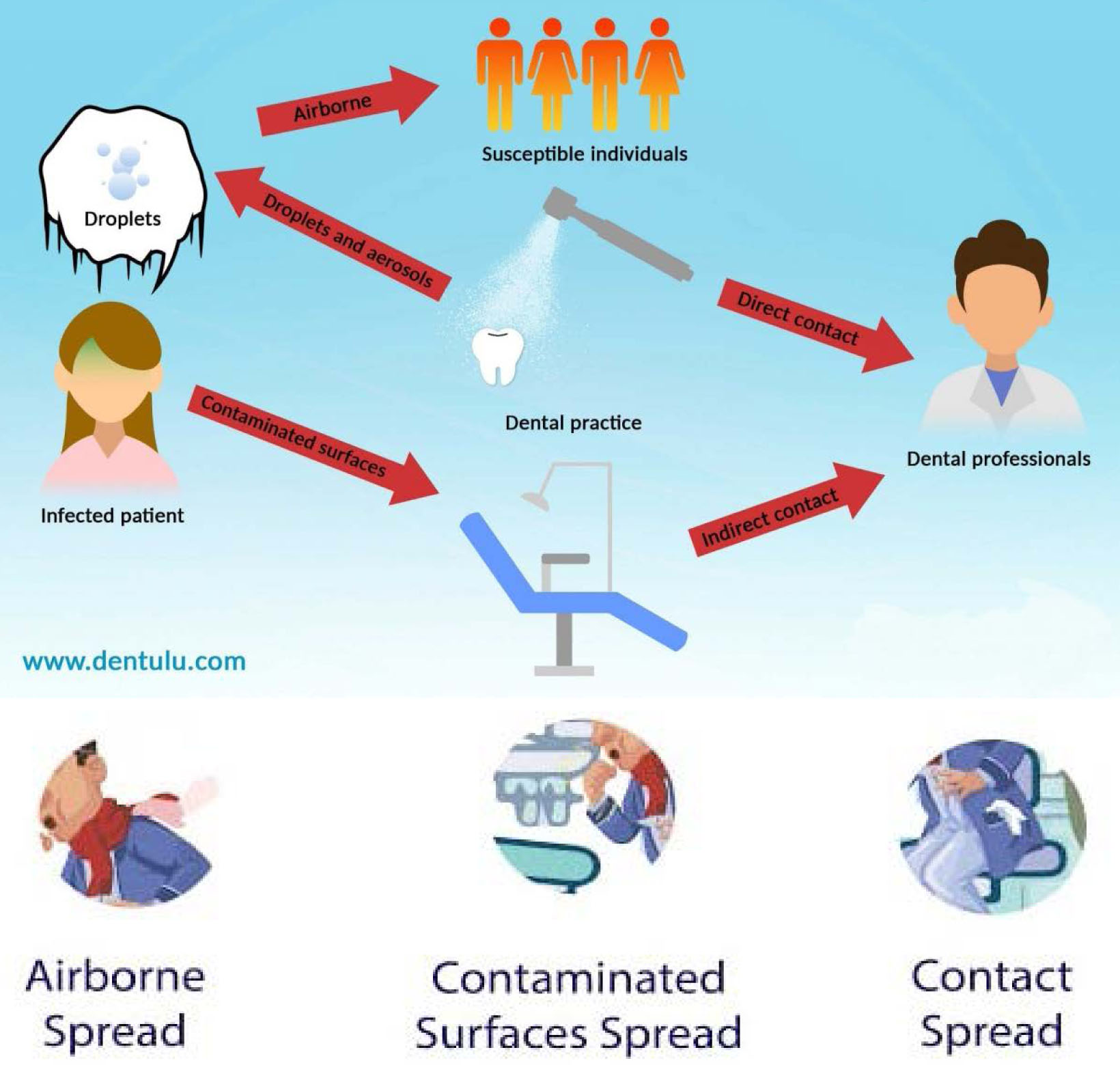
Due to the nature of the dental work and face-to-face communication, both patients and dental professionals are at the high risk of COVID-19 infection. In addition, frequent exposure to saliva, blood, and other body fluids, and the handling of sharp instruments during treatment and checking procedure further increase the risk of disease [7]. The transmission by contaminated blood should also be considered. In this context, health care workers, such as dentists, may be unknowingly providing direct care for infected, but not yet diagnosed COVID-19 patients [26]. Asymptomatic infections seem to be possible [16] and transmission may occur before the disease symptoms appear. The pathogenic microorganisms can be spread in dental settings through inhalation of airborne microorganisms that can remain suspended in the air for long periods [27]. Three possible routes for transmission of COVID-19 infection in dental clinic are given below.
- Airborne spread is well-reported in many literatures shows that many dental procedures produce aerosols and droplets that are contaminated with virus [28]. Thus, droplet and aerosol transmission of SARS-CoV-2 is the most important concern in dental clinics and hospitals, because it is hard to avoid the generation of large amounts of aerosol and droplet mixed with patient’s saliva and even blood during dental practice [29].
- Contact spread makes a possible route to the spread of viruses by dental professionals due to frequent direct or indirect contact with human fluids, patient materials, and contaminated dental instruments or environmental surfaces [7].
- Notable study of contaminated surfaces shows that SARS-CoV-2 can persist on surfaces like metal, glass, or plastic for up to a couple of days [27],[30]. Therefore, in health care settings contaminated surfaces that are frequently contacted are a potential source of coronavirus transmission. Droplets and aerosols from infected patients, which likely contaminate the whole surface in dental offices. From the studies of SARS-CoV-2, it was shown that at room temperature the CoV remains infectious from 2 hours up to 9 days. Especially during the outbreak of SARS-CoV-2, infections could be present through any of these conditions involved in an infected individual in dental clinics and hospitals (Figure 3) [7].
DENTAL PRACTICE RECOMMENDATIONS DURING COVID-19 OUTBREAK
- All nonessential and elective dental services are suspended immediately due to the specificity of its procedures, which involves face-to-face communication with patients, frequent exposure to saliva, blood, and other body fluids, and the handling of sharp instruments. In dental settings the pathogenic microorganisms can be transmitted through inhalation of airborne microorganisms that can remain suspended in the air for long periods. The latest update (March 16, 2020) by the American Dental Association (ADA) recommends dentists nationwide defer elective dental treatment for the next three weeks and focus on emergency care [7].
- Elective oral and maxillofacial surgery must be suspended immediately. A study by Lei et al. in Wuhan, China suggests that surgery may accelerate and exacerbate disease progression of COVID-19 during incubation period and poor prognosis of operative patients with fatal result [31].
- Emergency treatment should continue by block the person-to-person transmission routes in dental clinics and hospitals through infection control measures during dental practice [7].
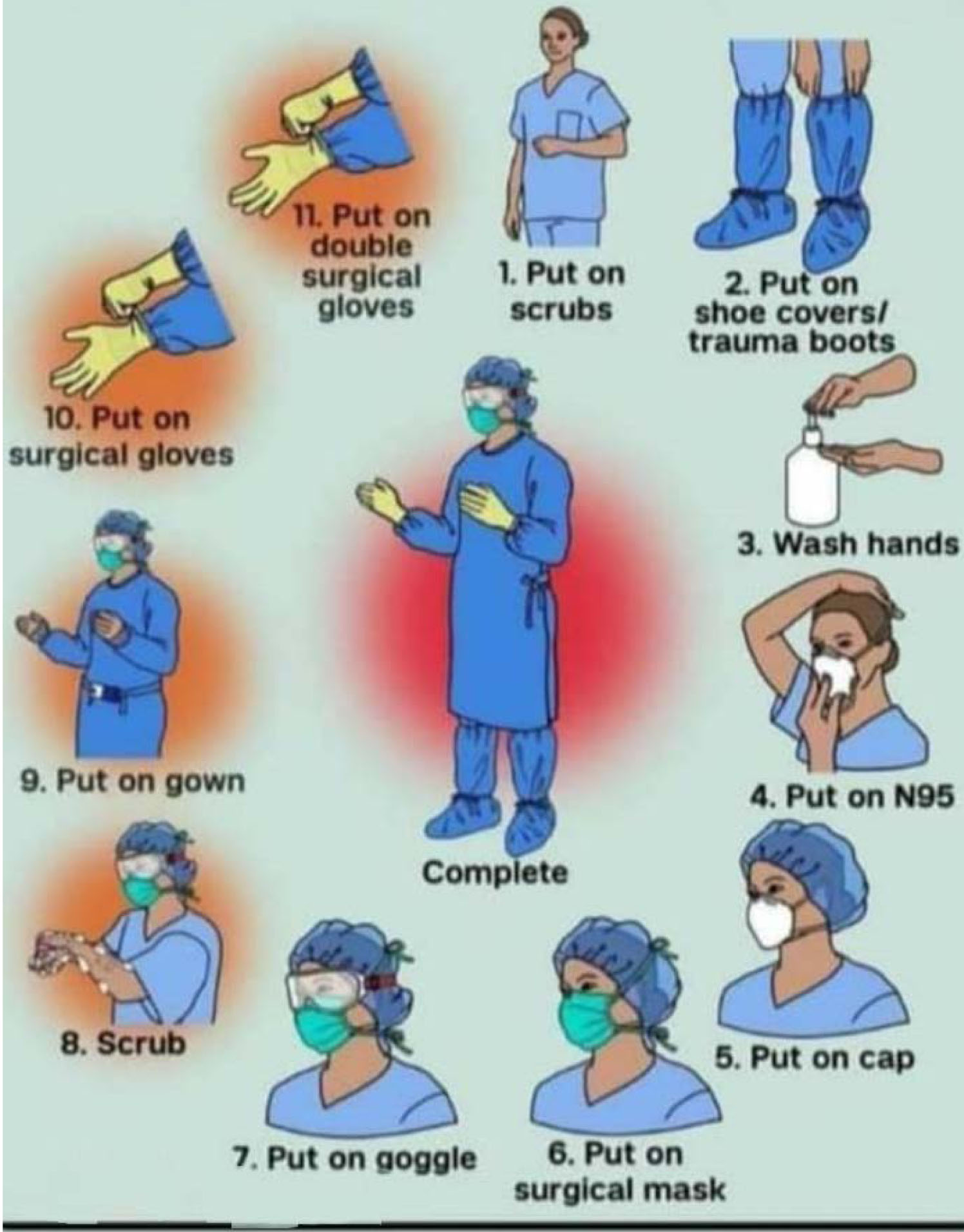
- Personal protective equipment (PPE) for dentists, dental professionals, and all dental staff. All must be wearing a disposable mask (N95), disposable gown, disposable latex gloves, disposable head cup, face shield protection, and impermeable shoe cover should be worn. The sequence of dressing PPE is shown in (Figure 4) [32].
- Good infection control measures should be followed by dental professionals, particularly considering the fact that aerosols and droplets were considered as the main spread routes of SARS-CoV-2 [33].
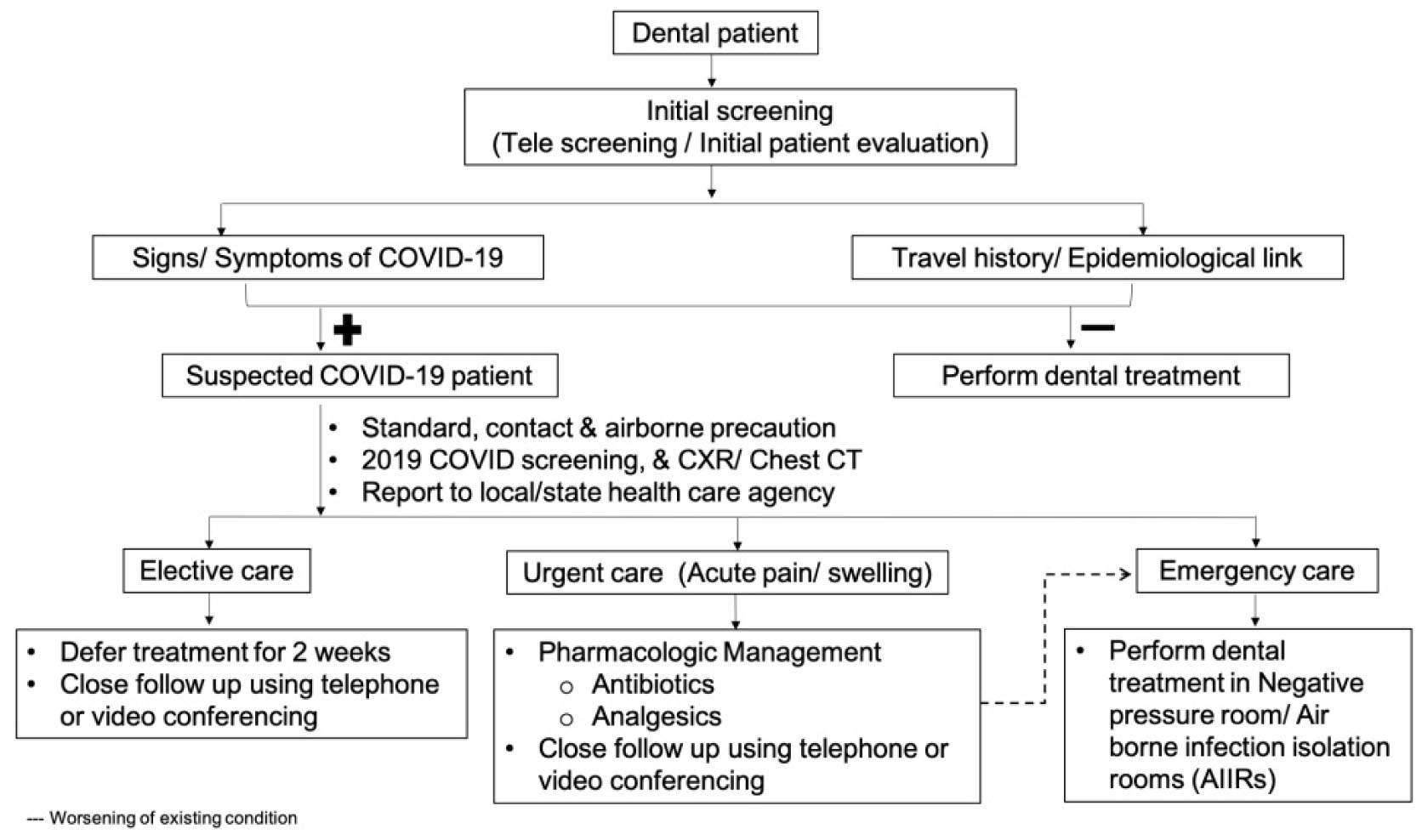
- All dental clinics are recommended to establish pre-check triages (Figure 5) during the outbreak of COVID-19 to measure and record the temperature of every staff and patient as a routine procedure. Pre-check staff should ask patients questions about the health status and history of contact or travel. Patients and their attendants are provided with medical masks and their temperature measurement must be below 37.3 °C once they enter into the hospital [32].
- Patients with fever should be registered and referred to designated hospitals. If a patient has been from epidemic regions (areas where COVID-19 spreads) within the past 14 days, quarantine for at least 14 days is suggested (Figure 5) [32].
- It was reported that dental practice should be postponed at least one month for convalescing patients with COVID-19 [2].
- Oral professionals should wash their hands before patient examination, before dental procedures, after touching the patient, after touching the surroundings and equipment without disinfection, and after touching the oral mucosa, damaged skin or wound, blood, body fluid, and secretion. Precaution should be taken by the dental professionals to avoid touching their own eyes, mouth, and nose [7].
- Mouth rinse before dental procedures is generally believed to reduce the number of oral microbes, especially mouth rinse containing oxidative agents. It has been suggested that the patient should perform a 1-min mouth rinse with 0.2–1% povidone, 0.05–0.1% cetylpyridinium chloride, or 1% hydrogen peroxide prior to the dental procedure for the purpose of reducing the salivary load of oral microbes, including potential SARS-CoV-2 carriage [33].
- Use of rubber dams means rubber dam isolation can significantly minimize the production of saliva-and blood-contaminated aerosol or spatter, particularly in cases when high-speed hand pieces and dental ultrasonic devices are used [32].
- Use (single use) disposable devices, such as turbine, mouth mirror, bur, and dental syringe to prevent cross infection and contamination [32].
- Extraoral radiograph such as panoramic radiograph or cone beam computed tomography (CBCT) is the best choice in comparison to intraoral radiograph, which makes gag reflex and cough to prevent cross infection and contamination [32].
- Patients with suspected or confirmed COVID-19 infection should not be treated in a routine dental practice background. In addition, patients should only be treated in negative pressure rooms or airborne infection isolation (AIIRs) [7].
- The staff should take effective and strict infection control measures in both dental clinic and public area, which should also be frequently cleaned and disinfected, such as door handles, chairs, and desks. Inside elevators, all people should wear masks correctly and avoid direct contact with buttons and other objects and the elevator should be disinfected regularly [2].
- Disposable protective equipment (all medical waste) after use should be transported to the temporary storage area of the medical institute also should be pretreated, cleaned, sterilized, and properly stored the reusable instrument and item [7].
CONCLUSION
The rapidly increasing number of cases and evidence of human-to-human transmission suggested that the virus was more contagious than SARS-CoV and MERS-CoV by mid-March 2020. A large number of infections of medical staff have been reported, health care professionals have the duty to protect the public and maintain high standards of care and infection control. Thus, it is important to make informed clinical decisions, educate the public to prevent panic while promoting the health and wellbeing of our patients during these challenging times. In this article, we also reviewed several detailed practical strategies to block virus transmission and suggest all nonessential and elective dental services are suspended immediately. Emergency treatment should continue with good infection control measures.
REFERENCES
1.
Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet 2020;395(10223):470–3. [CrossRef]
[Pubmed]

2.
Meng L, Hua F, Bian Z. Coronavirus disease 2019 (COVID-19): Emerging and future challenges for dental and oral medicine. J Dent Res 2020;99(5):481–7. [CrossRef]
[Pubmed]

3.
Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395(10223):497–506. [CrossRef]
[Pubmed]

4.
Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382(18):1708–20. [CrossRef]
[Pubmed]

5.
Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;323(11):1061–69. [CrossRef]
[Pubmed]

6.
Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). 2020. [Available at: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf]

7.
Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci 2020;12(1):9. [CrossRef]
[Pubmed]

8.
Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020;579(7798):270–3. [CrossRef]
[Pubmed]

9.
Gorbalenya AE, Baker SC, Baric RS, et al. Severe acute respiratory syndrome-related coronavirus: The species and its viruses – a statement of the Coronavirus Study Group. bioRxiv 2020;1–20. [CrossRef]

10.
Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020;382(8):727–33. [CrossRef]
[Pubmed]

11.
Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 2020;395(10224):565–74. [CrossRef]
[Pubmed]

12.
Perlman S. Another decade, another coronavirus. N Engl J Med 2020;382(8):760–2. [CrossRef]
[Pubmed]

13.
Tang X, Wu C, Li X, et al. On the origin and continuing evolution of SARS-CoV-2. National Science Review 2020;1–26. [CrossRef]

14.
Wu A, Peng Y, Huang B, et al. Genome composition and divergence of the novel coronavirus (2019-nCoV) originating in China. Cell Host Microbe 2020;27(3):325–8. [CrossRef]
[Pubmed]

15.
Shu Y, McCauley J. GISAID: Global initiative on sharing all influenza data – from vision to reality. Euro Surveill 2017;22(13). pii: 30494. [CrossRef]
[Pubmed]

16.
Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet 2020;395(10223):514–23. [CrossRef]
[Pubmed]

17.
Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med 2020;382(10):970–71. [CrossRef]
[Pubmed]

18.
Backer JA, Klinkenberg D, Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20–28 January 2020. Euro Surveill 2020;25(5). [CrossRef]
[Pubmed]

19.
Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med 2020;382(13):1199–207. [CrossRef]
[Pubmed]

20.
Xie X, Li Y, Sun H, Liu L. Exhaled droplets due to talking and coughing. J R Soc Interface 2009;6 Suppl 6:S703–14. [CrossRef]
[Pubmed]

21.
Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth 2020;67(5):568–76. [CrossRef]
[Pubmed]

22.
Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med 2020;382(10):929–36. [CrossRef]
[Pubmed]

23.
Yang Y, Lu Q, Liu M, et al. Epidemiological and clinical features of the 2019 novel coronavirus outbreak in China. medRxiv 2020;1–2. [CrossRef]

24.
World Health Organization. Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected: Interim guidance, 28 January 2020. World Health Organization. 2020. [Available at: https://who.int/iris/handle/10665/330893]

25.
Gamio L. The Workers Who Face the Greatest Coronavirus Risk. March 15, 2020. [Available at: https://www.nytimes.com/interactive/2020/03/15/business/economy/coronavirus-worker-risk.html?a ction=click&module=Top+Stories&pgtype=Homepage]

26.
World Health Organization. Global surveillance for COVID-19 disease caused by human infection with novel coronavirus (COVID-19): Interim guidance, 27 February 2020. World Health Organization. 2020. [Available at: https://apps.who.int/handle/10665/331231]

27.
Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect 2020;104(3):246–51. [CrossRef]
[Pubmed]

28.
Wei J, Li Y. Airborne spread of infectious agents in the indoor environment. Am J Infect Control 2016;44(9 Suppl):S102–8. [CrossRef]
[Pubmed]

29.
Cleveland JL, Gray SK, Harte JA, Robison VA, Moorman AC, Gooch BF. Transmission of blood borne pathogens in US dental health care settings: 2016 update. J Am Dent Assoc 2016;147(9):729–38. [CrossRef]
[Pubmed]

30.
Otter JA, Donskey C, Yezli S, Douthwaite S, Goldenberg SD, Weber DJ. Transmission of SARS and MERS coronaviruses and influenza virus in healthcare settings: The possible role of dry surface contamination. J Hosp Infect 2016;92(3):235–50. [CrossRef]
[Pubmed]

31.
Lei S, Jiang F, Xia ZY, Xia Z. Author's reply – clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine 2020:100363. [CrossRef]
[Pubmed]

32.
Ather A, Patel B, Ruparel NB, Diogenes A, Hargreaves KM. Coronavirus disease 19 (COVID-19): Implications for clinical dental care. J Endod 2020;46(5):584–95. [CrossRef]
[Pubmed]

33.
Izzetti R, Nisi M, Gabriele M, Graziani F. COVID-19 transmission in dental practice: Brief review of preventive measures in Italy. J Dent Res 2020:22034520920580. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Payman Kh Mahmud - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Shakhawan M Ali - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Dana Khdr Sabir - Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 Payman Kh Mahmud et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.