|
Technical Reports
The preservative confidentiality of formalin 10% on post-dental implant stability (in vitro study)
1 PhD, Lecturer, Department of OMFS, College of Dentistry, University of Mosul, Nineveh, Iraq
2 BDS, FIBMS (MF), Assistant Professor, Department of OMFS, College of Dentistry, University of Mosul, Nineveh, Iraq
3 BDS, MSc, Lecturer, Department of OMFS, College of Dentistry, University of Mosul, Nineveh, Iraq
Address correspondence to:
Alyaa I Naser
BDS, MSc, Lecturer, Department of OMFS, College of Dentistry, University of Mosul, Nineveh,
Iraq
Message to Corresponding Author
Article ID: 100041D01AA2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Aldabagh AHN, Deleme ZH, Naser AI. The preservative confidentiality of formalin 10% on post-dental implant stability (in vitro study). Edorium J Dent 2021;8:100041D01AA2021.ABSTRACT
Introduction: The dental implant steadiness has been estimated in clinical trials, but a precise amount is frequently tough in experimental simulations. In such circumstances, the amount of implant stability quotient (ISQ) inside the jawbone is desirable afterward formalin fixation.
Aim: This research aims to explore the influence of formalin 10% fixation on the implant stability.
Material and Methods: Twelve dental implants (Dentium Co. Ltd, Suwon, Korea) and four fresh natural tibia bones of sheep gained from the slaughter workshop had been utilized in this research, the implants inserted in the bone specimen then fixed in formalin 10%, and the ISQ was calculated employing device named Osstell mentor at day zero, day 10, day 30, day 60, and day 90.
Result: Implant stability quotient readings were showed no significant differences among evaluated times. Conclusions: These findings propose that bone fixation in formalin does not disturb the implant stability quotient after fixation in bone.
Keywords: Dental implant, Formalin, Preservative
INTRODUCTION
The density of osteal tissue is the chief element in influential points in dental implant steadiness [1],[2]. Which is then decided the success of the Osseo integrated process [3]. Its precise quantity earlier to implant appointment may permit the dental practitioner to modify spot grounding and realize suitable steadiness to weight the implant rendering to the finest procedure [4]. Another element that affects primary implant stability is the existence and width of a cortical bone layer that may, in turn, become a stable factor for implant since its structural and mechanical characteristics [5],[6],[7],[8]. The bone of the cortex shows important anatomical structures that shown by a bone of the core (cancellous) [8]. That arrangement provides suitable mechanical characteristics, with a better density and compressive power, and rigidity [7],[8],[9],[10]. These characteristics illustrate less subject unpredictability than those of marrow bone. “Formalin is an extremely reactive electrophilic chemical that reacts with tissues” [11],[12]. Implant stability quotient (ISQ) is a simple technique and easy handling for utilization in human and experimental animals [13],[14],[15], “which is an act by consuming resonance frequency analysis, that processes the emitting frequency over a vibration transducer contact to the fixture” [16],[17],[18]. To get maximum readings of ISQ we should fasten the transducer tightly to the implant fixture without any separating materials. In case of experimental models intervening media, we need formalin fixation of the specimen, after elimination of soft tissues. There is a fine possibility that “formalin fixation alter the ISQ by denaturing the protein in the bone,” as it is a widely available liquid for fixation, and “the formaldehyde contained in the formalin penetrates cells, where the aldehyde group in the molecule combines with nitrogen or some other atom in the organic fraction of the tissue for three hours” [19], also damage of the elasticity in osteal tissue as it terminates “the three-dimensional conformation of the present proteins by cross-linking their arrangements” [20],[21].
The purposes of this study are to assess the effectiveness of utilizing formalin 10% as a preservative media for specimens with a dental implant at different times by using implant stability as a parameter in clinical in vitro studies.
MATERIALS AND METHODS
Twelve dental implants (Dentium Co. Ltd, Suwon, Korea) and four fresh natural tibia bones of sheep obtained from the butcher workshop were utilized for this research. A 3 cm skin incision was done parallel to the long axis of the lateral surface of the tibia. The osteotomy site was prepared according to standard drilling protocol with a Dentium implant set with surgical instruments used as shown in Figure 1A and Figure 1B. Afterward, dissection of fascia was started, and the full-thickness flap was reflected, serial drilling was accomplished following system manufacturer’s references, i.e., preparation starts by Lindemann guide 2.2 mm drill followed by Lindemann first drill 2.6 mm then by final drill followed by countersink. Drilling was made intermittently as shown in Figure 1C. Three dental implants were (diameter 3.6 mm, length 10 mm) inserted in the tibia as shown in Figure 2A. At room temperature (25° C) normal saline solution was used as irrigating the place and to preserve the continuity throughout drilling by using the cooling system and at a constant ratio (40 mL/minute). The drill speed was fixed at 1062 rpm and the torque maintained at 50 n/cm (high dense bone), the gear ratio was 1:32, as shown in Figure 2B. Subsequently, a dental implant was installed manually until implant bodies submerged in bone, three dental implants were inserted in each bone. Then immediately after the insertion of dental implant and before immersing them in formalin (zero-day), the measurement of the primary stability was initiated by using osstell mentor as shown in Figure 2C by fixation of a transducer to the fixture (SmartPeg) by hand and tightened. Then “measurements probe was held close to the top of the smart peg.” At a distance of about 2 mm, the SmartPeg is stimulated by an attractive pulse from the probe readings. On the Osstell mentor screen, the outcome data are demonstrated. Implant stability quotient is estimated from the response signal. It is numbered from 1 to 100, the higher the readings the superior the steadiness. Implant stability quotient values were measured four times perpendicular to SmartPeg, and one time in parallel orientations to it (i.e., anterior, posterior, mesial, distal, and perpendicular). Moreover, the average was recorded as the final reading (1 was considered as least stable to 100 most stable). After that, the bone with the inserted implant was immersed in buffered 10% formalin as shown in Figure 1D and the same measurement protocol of primary stability was applied in ten days, one month, two months, and three months. Then data is statistically analyzed.
RESULTS
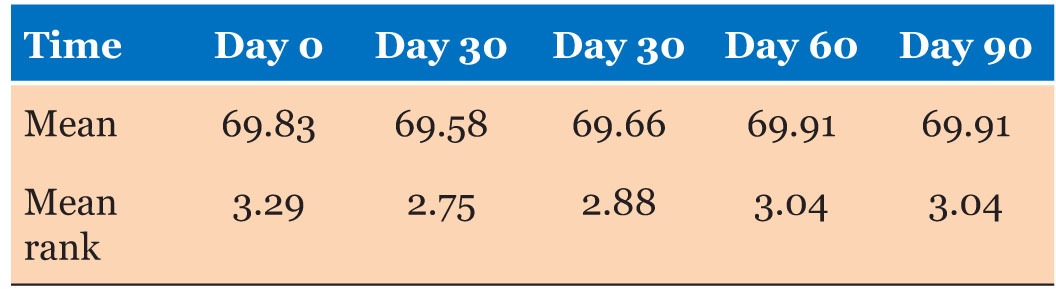
A non-parametric test was utilized to investigate the statistics and Friedman test applied to show there are no statistical differences among time of estimation of the specimens, in which Chi-square was 0.960 and p-value was 0.916 which means non-significant result as p-value is significant at ≤0.05. Table 1 shows the mean and mean rank by Friedman test of implant stability quotient according to days after immersed in formalin 10%.
DISCUSSION
Implant stability quotient has been extensively assessed in researches and in vitro studies but precise amount is frequently tough in vitro, so for that reason quantity of ISQ in osteal tissue is required afterward formalin fixation [22], Formaldehyde has three properties on tissue fragments—it penetrates cells, binds protein amino groups, and forms a bridge between the formalin and the protein. Bone hardens under its influence, and structural strength decreases [23]. The ISQ readings can be tested by the Osstell system and regarded as an efficient modality post-implant fixture placement which in turn considered as an indicator of stability [24]. Additionally, all implants with ISQ of more than 60 reached respectable stabilization of the hard tissue portion, which affects ISQ on that part (hard tissue portion). The influence of formalin showed no statistical significant difference, subsequently formalin considers to have the probable alteration of ISQ as it fixes the organic part of the peri-implant osteal tissue [25]. According to our findings, ISQ of an implant that is reinforced by the neighboring inorganic constituents of osteal tissue was not influenced by the lengthening time of preservation.
CONCLUSION
In conclusion, formalin fixation of osteal tissue may not influence ISQ in different times up to three months of storage of the specimen especially for academic purposes of master and doctorate implant researches and we can regard it as a good preservative media.
REFERENCES
1.
Marquezan M, Osório A, Sant’Anna E, Souza MM, Maia L. Does bone mineral density influence the primary stability of dental implants? A systematic review. Clin Oral Implants Res 2012;23(7):767–74. [CrossRef]
[Pubmed]

2.
Molly L. Bone density and primary stability in implant therapy. Clin Oral Implants Res 2006;17 Suppl 2:124–35. [CrossRef]
[Pubmed]

3.
Javed F, Ahmed HB, Crespi R, Romanos GE. Role of primary stability for successful osseointegration of dental implants: Factors of influence and evaluation. Interv Med Appl Sci 2013;5(4):162–7. [CrossRef]
[Pubmed]

4.
Javed F, Romanos GE. The role of primary stability for successful immediate loading of dental implants. A literature review. J Dent 2010;38(8):612–20. [CrossRef]
[Pubmed]

5.
Howashi M, Tsukiyama Y, Ayukawa Y, et al. Relationship between the CT value and cortical bone thickness at implant recipient sites and primary implant stability with comparison of different implant types. Clin Implant Dent Relat Res 2016;18(1):107–16. [CrossRef]
[Pubmed]

6.
Hong J, Lim YJ, Park SO. Quantitative biomechanical analysis of the influence of the cortical bone and implant length on primary stability. Clinical of Oral Implants Research 2012;23(10):1193–7. [CrossRef]

7.
8.
9.
Robertson DM, Smith DC. Compressive strength of mandibular bone as a function of microstructure and strain rate. J Biomech 1978;11(10–12):455–71. [CrossRef]
[Pubmed]

10.
Schaffler MB, Burr DB. Stiffness of compact bone: Effects of porosity and density. J Biomech 1988;21(1):13–6. [CrossRef]
[Pubmed]

11.
Rho JY, Kuhn-Spearing L, Zioupos P. Mechanical properties and the hierarchical structure of bone. Med Eng Phys 1998;20(2):92–102. [CrossRef]
[Pubmed]

12.
Cömert A, Kökat AM, Akkocaoglu M, Tekdemir I, Akça K, Cehreli MC. Fresh-frozen vs. embalmed bone: Is it possible to use formalin-fixed human bone for biomechanical experiments on implants? Clin Oral Implants Res 2009;20(5):521–5. [CrossRef]
[Pubmed]

13.
Abtahi J, Tengvall P, Aspenberg P. A bisphosphonate-coating improves the fixation of metal implants in human bone. A randomized trial of dental implants. Bone 2012;50(5):1148–51. [CrossRef]
[Pubmed]

14.
Gottlow J, Barkarmo S, Sennerby L. An experimental comparison of two different clinically used implant designs and surfaces. Clin Implant Dent Relat Res 2012;14 Suppl 1:e204–12. [CrossRef]
[Pubmed]

15.
Palarie V, Bicer C, Lehmann KM, Zahalka M, Draenert FG, Kämmerer PW. Early outcome of an implant system with a resorbable adhesive calcium-phosphate coating—a prospective clinical study in partially dentate patients. Clin Oral Investig 2012;16(4):1039–48. [CrossRef]
[Pubmed]

16.
Xiao JR, Li YQ, Guan SM, Kong L, Liu B, Li D. Effects of lateral cortical anchorage on the primary stability of implants subjected to controlled loads: An in vitro study. Br J Oral Maxillofac Surg 2012;50(2):161–5. [CrossRef]
[Pubmed]

17.
De Santis E, Botticelli D, Pantani F, Pereira FP, Beolchini M, Lang NP. Bone regeneration at implants placed into extraction sockets of maxillary incisors in dogs. Clin Oral Implants Res 2011;22(4):430–7. [CrossRef]
[Pubmed]

18.
Isoda K, Ayukawa Y, Tsukiyama Y, Sogo M, Matsushita Y, Koyano K. Relationship between the bone density estimated by cone-beam computed tomography and the primary stability of dental implants. Clin Oral Implants Res 2012;23(7):832–6. [CrossRef]
[Pubmed]

19.
Kim SK, Lee HN, Choi YC, Heo SJ, Lee CW, Choie MK. Effects of anodized oxidation or turned implants on bone healing after using conventional drilling or trabecular compaction technique: Histomorphometric analysis and RFA. Clin Oral Implants Res 2006;17(6):644–50. [CrossRef]
[Pubmed]

20.
Currey JD, Brear K, Zioupos P, Reilly GC. Effect of formaldehyde fixation on some mechanical properties of bovine bone. Biomaterials 1995;16(16):1267–71. [CrossRef]
[Pubmed]

21.
Goh JC, Ang EJ, Bose K. Effect of preservation medium on the mechanical properties of cat bones. Acta Orthop Scand 1989;60(4):465–7. [CrossRef]
[Pubmed]

22.
Morita K, Doi K, Oue H, Kajihara S, Hayashi K, Akagawa Y. Influence of formalin fixation on the implant stability quotient and mechanical characteristics of bone. Br J Oral Maxillofac Surg 2013;51(6):550–4. [CrossRef]
[Pubmed]

23.
Rouleau L, Tremblay D, Cartier R, Mongrain R, Leask RL. Regional variations in canine descending aortic tissue mechanical properties change with formalin fixation. Cardiovasc Pathol 2012;21(5):390–7. [CrossRef]
[Pubmed]

24.
Al-Khaldi N, Sleeman D, Allen F. Stability of dental implants in grafted bone in the anterior maxilla: longitudinal study. Br J Oral Maxillofac Surg 2011;49(4):319–23. [CrossRef]
[Pubmed]

25.
Miyamoto I, Tsuboi Y, Wada E, Suwa H, Iizuka T. Influence of cortical bone thickness and implant length on implant stability at the time of surgery— clinical, prospective, biomechanical, and imaging study. Bone 2005;37(6):776–80. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Abdul Hameed N Aldabagh - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ziad H Deleme - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Alyaa I Naser - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Abdul Hameed N Aldabagh et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.