|
Research Article
The effect of “Alveolex” in preventing of alveolar ostitis associated with extraction of lower molar teeth in Mosul dental teaching hospital
1 Assistant Lecturer, Oral and Maxillofacial Surgery Department, Dentistry College, Mosul University, Mosul, Iraq;
2 Lecturer, Oral and Maxillofacial Surgery Department, Dentistry College, Mosul University, Mosul, Iraq
Address correspondence to:
Noor A Sulaiman
Al-Muthannaa Street, Mosul,
Iraq
Message to Corresponding Author
Article ID: 100045D01WM2023
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Mahmood WK, Sulaiman NA, Al-Jewari SSA. The effect of “Alveolex” in preventing of alveolar ostitis associated with extraction of lower molar teeth in Mosul dental teaching hospital. Edorium J Dent 2023;10(1):1–6.ABSTRACT
Aim: To evaluate the validity of new material in avoiding dry socket development after tooth extraction in suspected cases.
Methods: 169 patients counted in this study, attended for lower molars extraction due to different reasons, having predisposing factors of dry socket development post-extraction, divided into two groups, control group (87 patients) with extraction socket left without treatment and, a study group (82 patient) treated by “Alveolex” material placed in the socket directly after extraction. Post-operative clinical evaluation for dry socket development in both groups has been performed.
Results: Control group showed more females affected with dry sockets than males. Dry socket developed more in smoker males whose sockets were left without treatment, also females who took contraceptive pills showed more dry socket in control, while all the patients have no dry socket at all in the study group regardless of the gender, smoking, or contraceptive pills taking.
Conclusion: Topical application of (Alveolex) after dental extraction prevents dry socket formation.
Keywords: Alveolex, Alveolar ostitis, Dry socket, Propolis
INTRODUCTION
One of the most common problems following dental extraction is a dry socket which has various names like alveolar osteitis [1]. Characterized by severe pain at extraction site 2–4 days later, clinically appear as empty socket without clot but filled by food debris and surrounded by red inflamed congested gingiva with or without fetid odor. It occurs more in 4th decade of life, with incidence of 1–4% increased to 5–30% following third molars extraction, it has been found that mandibular molar teeth associated with dry socket are about 10 times more affected than maxillary molars, and females are more affected than males with a ratio of 8.2:1 [2],[3].
Despite the exact cause is still unknown, it has been found that the fibrinolytic activity of bacterial enzymes prevents clot creation and leads to dry socket. Knowledge of the risk factors, accurate treatment planning, and patient preparation are essential to prevent this problem [4]. There are many risk factors including lower teeth, female, young adult, contraceptive pills, smoking, poor oral hygiene, infection, difficult prolonged extraction, high dose of local anesthesia, repeated sucking, rinsing, or spitting after extraction, inexperienced operator [5],[6]. It has been established that the management strategies of dry socket commonly depend on professionals’ views and clinical experience despite there is no strong proof related to its efficiency, which includes multiple follow-up visits [5],[6].
Various therapeutic agents have been used to decrease the occurrence of dry sockets like antibiotics, antiseptics, anti-inflammatory agents, antifibrinolytics, and lately plasma rich in growth factors. Using antibiotics systematically does not remove the threat of dry socket, even may lead to bacterial resistance, furthermore, antiseptics, anti-inflammatory, and analgesics drugs do not absolutely diminish pain and swelling, so to reduce these problems, local interventions have been used, although there is no proof supporting any of these methods. So, it is compulsory to find new treatments able to decrease or prevent the occurrence of dry socket [6].
One of these treatment approaches relies on natural products owing to it being safe and cost-effective. Among natural products that are used as a medicine for specific illnesses in various ancient cultures is Propolis, defined as bee affix, a multifarious material, formed by bees to preserve them from bacterial or fungal contaminations and to seal any clefts in hives [7].
It comprises several elements and components gathered by bees from different plant greeneries, blossoms, and exudates. Broken down by enzymes of bee saliva and blended with beeswax, these are 50% of plant resin that include a large portion of Flavonoids which are considered the vigorous factor of propolis and related to the most of antibacterial, anti-oxidative, anticariogenic, antiviral, antifungal and anti-inflammatory features of propolis, 30% beeswax, 10% essential oils, 5% pollen, 5% organic substances, and different proportion of carbohydrates according to the type of propolis. It also has aromatic compounds, heavy metals (Cd, Hg, and Pb), vitamins (B1, B2, B6, C, and E), amino acids, resulting from the digestions of bees, and mineral elements (Mg, Ca, I, K, Na, Cu, Zn, Mn, and Fe) [8],[9].
Propolis has numerous therapeutic activities like anti-bacterial, anti-inflammatory, anti-viral, and anti-oxidant which is stronger than that of vitamin C, anti-protozoal, anesthetic, anti-tumoral, anti-cancer, anti-fungal, antiseptic, anti-mutagenic, anti-hypertensive, anti-hepatotoxic, and anti-cytotoxic action [8],[9].
We assumed that using the (Alveolex) following dental extraction will prevent dry socket formation in cases with predisposing factors for dry socket development.
MATERIAL AND METHOD
The schedule of this study was approved by the Scientific Committee of Dentistry College in Mosul University on 25/11/2019, the code no. is 584.
Inclusion criteria: patients above 18 years old with exclusively lower molar teeth need an extraction, female who is taking contraceptive pills for birth control or for gynecological reasons, heavy smoker male patients (more than 15 cigarettes per day), prolonged difficult traumatic extraction of a lower molar (need more than 30 minutes for extraction or need sectioning or splitting of the roots), and impacted wisdom teeth (surgical removal).
Exclusion criteria: allergy to honey or any component of it, seasonal allergy, and asthmatic patient.
According to the specific inclusion and exclusion criteria, the study includes 169 patients who attended teaching hospitals in dentistry college who need extraction of lower molar teeth exclusively due to different causes (un-restorable tooth, orthodontic, periodontal, impaction, etc.) having predisposing factors of dry socket development.
The Alveolex paste is from Biodinâmica International Company, Brazil. In 2×3 g syringes with applicable disposable tips composed of Propolis (10%), Iodoform (5%), Beeswax, Thickener.
Verbal consent has been taken from all patients and extraction done by the same operator. The patients were divided into two groups (control and study) containing smoker males and females with contraceptive pills, control group included 87 patients in which the socket was left without any treatment, while the study group contained 82 patients in which alveolex paste was applied by syringe and filled the socket after extraction totally, then covered by cotton, follow-up with clinical assessment was done for 2–4 days after extraction to detect any sign or symptoms of dry socket development in both groups.
Data analysis
All data appear as descriptive data, the analysis has been done by IBM SPSS Statistics version 25.0 statistical program. Descriptive statistical analysis between two groups was done by chi-square test and differences were considered significant at p = 0.01.
RESULTS
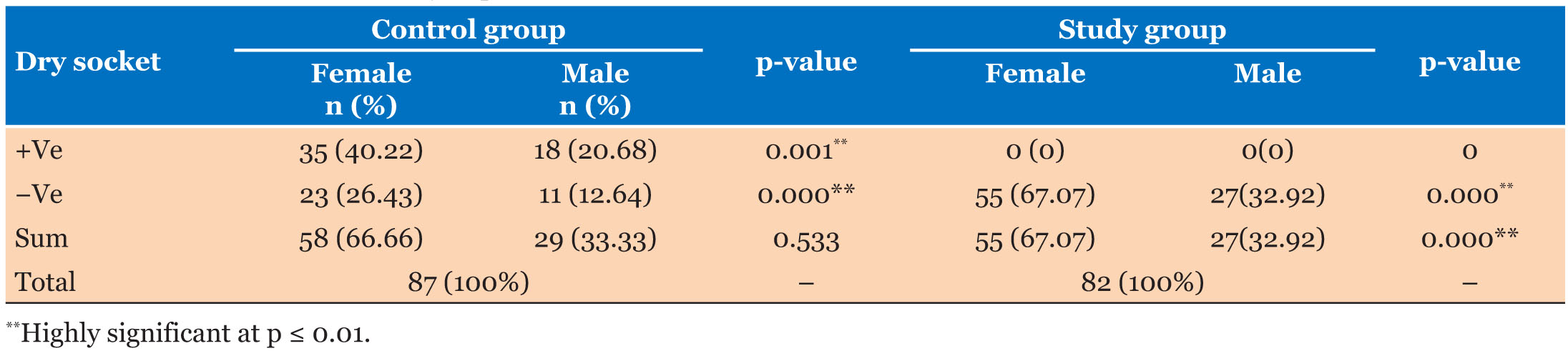
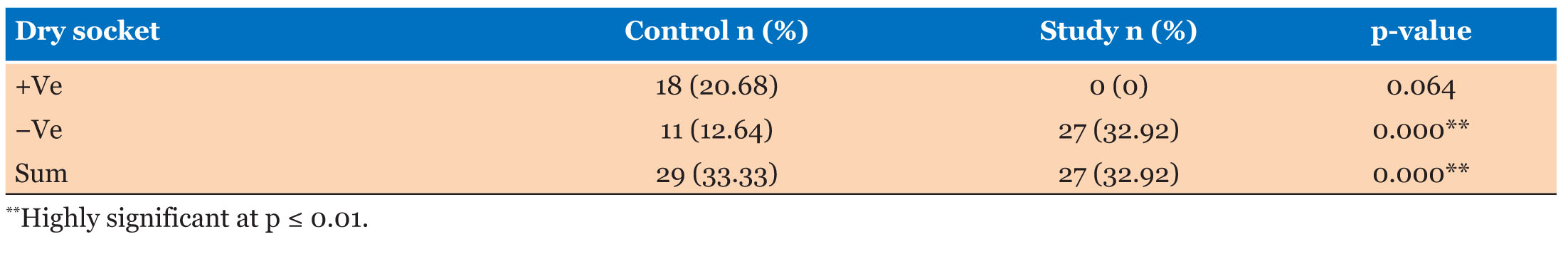
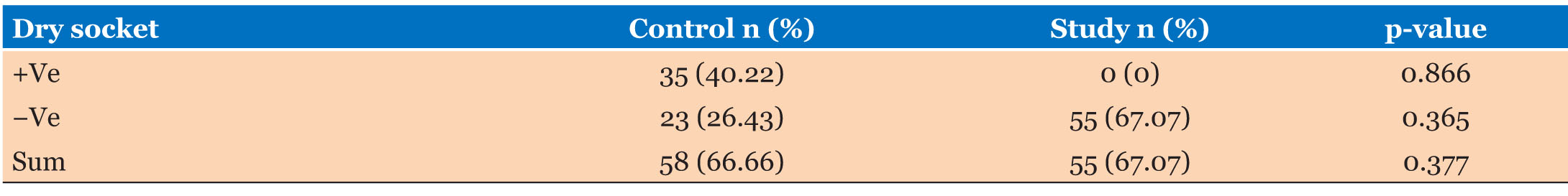
Our results revealed that dry socket is more common in females (35) than males (18) in the control group while all the patients have no dry socket in the study group regardless to the gender, in smoker males specifically only (11) patient has no dry socket in the control group while smoker males in the study group have no signs or symptoms of dry socket following extraction entirely. In females who were taking contraceptive pills, dry socket appeared in 35 females in the control group with no cases of dry socket are seen in the study group. All results shown in Table 1, Table 2, Table 3.
DISCUSSION
Dry socket is a self-limiting condition but accompanied by pain that affects the daily activities, with the poor effect of analgesic or narcotic treatments [3] . Various treatment modalities are present and different materials are applied to reduce or even prevent its occurrence.
Propolis has several therapeutic properties, such as anti-inflammatory, antibacterial, antifungal, analgesic, and healing properties, which considered the reason of use it in the medical and dental fields. It has been shown that it motivates bone regeneration through inhibiting osteoclastic activity, and uses as a bone-grafting substitute for the treatment of periodontal defects [6].
In our study, we used alveolex topical material after the extraction of lower molars to compare the incidence of dry socket between two groups of patients having predisposing factors for the development of dry socket. In this study, the control group showed a high presence of alveolar osteitis in female than the male which was highly significant in differences as female gender considered as a predisposing factor of dry socket, as they pass through a menstrual period which alters the level of estrogen that plays a role in the physiological condition of the body, which disturbs normal healing process. While the study group showed no case of dry socket in both genders. The same results were seen in Momeni et al. 2011, who included 4779 patients in their study, and studied many features that prompt the production of dry socket, such as age, sex, extraction position, smoking, oral contraceptive pill intake, and other factors. They mentioned that alveolar osteitis presented in higher prevalence in females than males (0.08% versus 0.04) [10]. Sweet and Butler 1977 also revealed that dry socket was present in 4.1% of female patients, while 0.5% in males [11]. Tjernberg stated that dry socket occurrence increased about 5-folds in female gender [12]. Also, MthethwaI and Mabhoza (2016) found that dry socket developed more in females and suggested a possible impact of hormonal variances between male and female [5].
Our results showed that dry socket increased in smoker males in the control group because negative pressure during smoking led to clot dislodgement, in addition to the effect of nicotine on the action of neutrophil and inflammatory reaction of the body. This goes with Rakhshan (2018), who stated that smoking could destruct healing, as clot suctioning disturbs blood vessels and leads to a decrease in blood stuffing of the socket, which increases the occurrence of alveolar osteitis. The exact method is still not clear although it could be related to cytotoxic elements such as nicotine, cotinine, carbon monoxide, and hydrogen cyanide. Nicotine acts as a vasoconstrictor when absorbed by the oral mucosa and causes catecholamine release with an increase in sticking of platelet leading to ischemia of tissue, in addition, the heat, and socket contaminants by smoking byproducts could prevent the healing mechanism [4]. Our results are compatible with other results as Eshghpour and Nejat (2013) pronounced a higher occurrence of dry socket in smokers, particularly after 24 hours from extraction [13]. Halabi et al. stated that the prevalence of dry socket raised significantly in patients who smoke a minimum of 5 cigarettes per day [14]. Again no cases of dry socket were present at all in the study group despite the presence of smoking factor in current study.
The present study revealed that females who take contraceptive pills in the control groups develop dry socket more than those who do not taken pills. These results are associated with the pills themselves as they cause an increase in estrogen levels that raise fibrinolysis of plasma. It has been documented that extra estrogen in oral contraceptives could increase plasma fibrinolysis [4]. This study agreed with Eshghpour et al. (2013), who found an increase in dry socket occurrence in women who used up these drugs due to a higher fibrinolytic activity caused by the drug [15]. Similarly, Mudali and Mahomed (2016) acted on more than 2000 patients needing surgical removal of lower third molar and established that dry socket present in 71.4% of females who are using oral contraceptives [16]. Almeida et al. (2016) studied the incidences of dry socket development in patients who presented with bilateral impacted lower wisdoms and classified them according to oldness, gender, and females with contraceptive pills. They cited that risk of dry socket formation increased by about 3.5 times in females consuming contraceptive pills [17]. Bhujbal et al. (2019) also recognized that alveolar osteitis occurs in women having oral contraceptives more than in women who were not [3] . While the group with alveolex showed no case of dry socket totally in our results.
As we previously mentioned in this study all cases treated by alveolex do not develop dry socket even with the presence of formerly cited risk factors, this can be associated with the structure of alveolex which include Propolis which clarified by much research that it has a number of medicinal actions. Propolis contains components (such as vitamin C, bioflavonoids, B complex, arginine, pro-vitamin A, and certain minerals) that have several therapeutic activities on tissue regeneration, because of its anti-inflammatory, antimicrobial, and immunomodulation properties. Additionally, it decreases the number of free radicals (anti-oxidant action) due to the presence of phenolic components and flavonoids, hastens various enzymatic reactions, blood circulation, cell metabolism, and raises collagen production [18],[19]. The results were highly significant in a difference between the control and study groups, these results agreed with Serrano et al. (2021), who used Propolis in dental sockets following impacted third molars extraction and stated that application of Propolis may be helpful in avoiding dry socket formation [6]. It has been found that Propolis reduces nuclear factor-?B (NF-?B) formation and blocking its action, so prevents ubiquitin units formation and anti-inflammatory actions [20]. Ansari et al. (2019) used honey for treatment of dry socket and stated that there was significant decrease in inflammation, and hyperemia, which causes decrease in the patients pain and discomfort [21]. Previous studies documented that Propolis extract has small pain killing effects and histological investigations showed ability to increase epithelialization rate when applied topically to dental socket and wounds of skin [22]. In future, this research can assist dentists to work freely in the extraction of the lower molars of any case with predisposing factors without any worriedness for dry socket development, and can avoid the patient from pain and unpleasant consequences of dry socket.
CONCLUSION
Topical application of (Alveolex) following dental extraction in patients with predisposing factors prevents dry socket formation. It is easily applicable, cost-effective, and can be used safely in a non-allergic patient with high acceptance by patients.
REFERENCES
1.
Taberner-Vallverdú M, Sánchez-Garcés MÁ, Gay-Escoda C. Efficacy of different methods used for dry socket prevention and risk factor analysis: A systematic review. Med Oral Patol Oral Cir Bucal 2017;22(6):e750–8. [CrossRef]
[Pubmed]

2.
Blum IR. Contemporary views on dry socket (Alveolar osteitis): A clinical appraisal of standardization, aetiopathogenesis and management: A critical review. Int J Oral Maxillofac Surg 2002;31(3):309–17. [CrossRef]
[Pubmed]

3.
4.
Rakhshan V. Common risk factors of dry socket (alveolitis osteitis) following dental extraction: A brief narrative review. J Stomatol Oral Maxillofac Surg 2018;119(5):407–11. [CrossRef]
[Pubmed]

5.
6.
González-Serrano J, López-Pintor RM, Cecilia-Murga R, Torres J, Hernández G, López-Quiles J. Application of propolis extract, nanovitamin C and nanovitamin E to prevent alveolar osteitis after impacted lower third molar surgery. A randomized, double-blind, split-mouth, pilot study. Med Oral Patol Oral Cir Bucal 2021;26(2):e118–25. [CrossRef]
[Pubmed]

7.
Elnakady YA, Rushdi AI, Franke R, et al. Characteristics, chemical compositions and biological activities of propolis from Al-Bahah, Saudi Arabia. Sci Rep 2017;7:41453. [CrossRef]
[Pubmed]

8.
Abbasi AJ, Mohammadi F, Bayat M, et al. Applications of propolis in dentistry: A review. Ethiop J Health Sci 2018;28(4):505–12. [CrossRef]
[Pubmed]

9.
Zaccaria V, Curti V, Di Lorenzo A, et al. Effect of green and brown propolis extracts on the expression levels of microRNAs, mRNAs and proteins, related to oxidative stress and inflammation. Nutrients 2017;9(10):1090. [CrossRef]
[Pubmed]

10.
Momeni H, Shahnaseri S, Hamzeheil Z. Evaluation of relative distribution and risk factors in patients with dry socket referring to Yazd dental clinics. Dent Res J (Isfahan) 2011;8(Suppl 1):S84–7.
[Pubmed]

11.
Sweet JB, Butler DP. Increased incidence of postoperative localized osteitis in mandibular third molar surgery associated with patients using oral contraceptives. Am J Obstet Gynecol 1977;127(5):518–9. [CrossRef]
[Pubmed]

12.
Tjernberg A. Influence of oral hygiene measures on the development of alveolitis sicca dolorosa after surgical removal of mandibular third molars. Int J Oral Surg 1979;8(12):430–4. [CrossRef]
[Pubmed]

13.
Eshghpour M, Nejat AH. Dry socket following surgical removal of impacted third molars in an Iranian population: Incidence and risk factors. Niger J Clin Pract 2013;16:496–500. [CrossRef]
[Pubmed]

14.
Halabí D, Escobar J, Munoz C, Muñoz S. Logistic regression analysis of risk factors for the development of alveolar osteitis. J Oral Maxillofac Surg 2012;70(5):1040–4. [CrossRef]
[Pubmed]

15.
Eshghpour M, Rezaei NM, Nejat A. Effect of menstrual cycle on frequency of alveolar osteitis in women undergoing surgical removal of mandibular third molar: A single-blind randomized clinical trial. J Oral Maxillofac Surg 2013;71(9):1484–9. [CrossRef]
[Pubmed]

16.
17.
Almeida LE, Pierce S, Klar K, Sherman K. Effects of oral contraceptives on the prevalence of alveolar osteitis after mandibular third molar surgery: A retrospective study. Int J Oral Maxillofac Surg 2016;45(10):1299–302. [CrossRef]
[Pubmed]

18.
Anjum SI, Ullah A, Khan KA, et al. Composition and functional properties of propolis (bee glue): A review. Saudi J Biol Sci 2019:26(7):1695–703. [CrossRef]
[Pubmed]

19.
Dantas Silva RP, Machado BAS, Barreto GDA, et al. Antioxidant, antimicrobial, antiparasitic, and cytotoxic properties of various Brazilian propolis extracts. PLoS One 2017;12(3):e0172585. [CrossRef]
[Pubmed]

20.
Aminimoghadamfarouj N, Nematollahi A. Propolis diterpenes as a remarkable bio-source for drug discovery development: A review. Int J Mol Sci 2017;18(6):1290. [CrossRef]
[Pubmed]

21.
Ansari A, Joshi S, Garad A, Mhatre B, Bagade S, Jain R. A study to evaluate the efficacy of honey in the management of dry socket. Contemp Clin Dent 2019;10(1):52–5. [CrossRef]
[Pubmed]

22.
Magro Filho O, de Carvalho AC. Application of propolis to dental sockets and skin wounds. J Nihon Univ Sch Dent 1990;32(1):4–13. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgments
Authors thank all the members of the Oral and Maxillofacial Surgery Department of Dentistry College, Mosul University.
Author ContributionsWaseem Khalid Mahmood - Conception of the work, Design of the work, Acquisition of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Noor A Sulaiman - Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Saif Saad Ali Al-Jewari - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2023 Waseem Khalid Mahmood et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.